Metabolic syndrome — (Reaven syndrome) is a symptom complex that combines abdominal obesity, insulin resistance, hyperglycemia (increased blood glucose), dyslipidemia and hypertension
All these disorders are connected in one pathogenetic chain. In addition, this syndrome is often combined with hyperuricemia (excess uric acid in the blood), impaired hemostasis (blood clotting), subclinical inflammation, obstructive sleep apnea-hypopnea syndrome (respiratory arrest during sleep).
Metabolic syndrome in women of reproductive age was previously known by practitioners as neurotransmission endocrine syndrome, occurring as a mild form of Cushing's disease, hypothalamic or diencephalic syndrome. In this article, the material will be presented from the perspective of a gynecologist- endocrinologist. In women of reproductive age, metabolic syndrome is one of the most common causes of reproductive dysfunction against the background of progressive obesity and diencephalic symptoms.
EPIDEMIOLOGY
The frequency of this pathology is up to 15- 20% in the population, about 30-35% in the structure of reproductive disorders and up to 70% among women with recurrent endometrial hyperplastic processes; the frequency of early pregnancy losses in this syndrome increases to 35%.
ETIOLOGY
The causes of the development of metabolic syndrome are the effects of various factors (mental stress, neuroinfections, various operations, injuries, childbirth, abortions, etc.) in women with a certain premorbid background (congenital or acquired functional lability of hypothalamic and extrahypothalamic structures).
PATHOGENESIS
Primarily, there is a violation of the neuroendocrine regulation of the hypothalamus, therefore, there are many diencephalic symptoms (sleep disorders, appetite, thirst, dizziness, headaches, hypertension, etc.), indicating the central (hypothalamic) genesis of this pathology. In response to the effects of various etiological factors (stress), neurotransmitter metabolism is disrupted in the extrahypothalamic structures of the brain, in particular, an increase in the synthesis and release of ?- endorphin and a decrease in dopamine production.
As a result, the secretion of ACSH (adrenocorticosteroid hormone) and prolactin increases, and the cyrhoral rhythm of gonadoliberin and, accordingly, gonadotropins in the pituitary gland is disrupted. Estrone, which is non-gonadally synthesized from androgens, increases the sensitivity of the pituitary gland to gonadoliberin, which additionally disrupts the function of the hypothalamic-pituitary- ovarian system with the formation of secondary polycystic ovaries.
Disorders in the hypothalamus-pituitary- adrenal gland system. In response to excessive stimulation of ACSH in the adrenal glands, the formation of all steroid hormones of the cortex increases: glucocorticoids (cortisol), mineralocorticoids (aldosterone) and sex hormones, mainly androgens.
Hypercorticism contributes to specific, so- called visceral obesity (central, cushingoid, male, android obesity) with predominant deposition of adipose tissue in the shoulder girdle, abdomen and mesentery of internal organs.
Visceral adipose tissue leads to the formation of insulin resistance due to hyperinsulinemia. Then there is a violation of the blood lipid spectrum (dyslipidemia), characterized by an increase in the level of atherogenic factors (triglycerides, low-density lipoproteins, very low-density lipoproteins) and a decrease in the level of high-density lipoproteins, which leads to atherosclerosis and arterial hypertension. In this case, the sequence of development of metabolic disorders corresponds to the duration of the disease.
Therefore, arterial hypertension, an obligatory component of the metabolic syndrome, usually manifests itself after the age of 35.
Visceral obesity is also promoted by bulimia (increased appetite and excessive food intake) due to impaired neurotransmitter control over the function of the centers of eating behavior located in the hypothalamus. Peripheral insulin resistance is also promoted by adrenal androgens and testosterone produced in adipose tissue. Androgens are known to alter the structure of muscle tissue towards the predominance of type II muscle fibers, which are less sensitive to insulin.
Thus, as a result of activation of the hypothalamus-pituitary-adrenal axis, 4 main components ("deadly quartet") of the metabolic syndrome are formed: visceral obesity, insulin resistance, dyslipidemia and arterial hypertension.
There is no clear classification and staging of the metabolic syndrome. Despite this, the severity of symptoms, the number of components of Raven syndrome and the presence of complications influence the risk stratification and the choice of treatment tactics in a particular patient. To do this, consider:
• the degree of obesity and hypertension;
• severity of metabolic changes;
• the presence or absence of diabetes mellitus and atherosclerosis-related diseases.
Depending on the body mass index (BMI), which is calculated by dividing weight (kg) by height (m2), the following types of body weight (MT) are classified:
• normal MT — BMI ?18.5 <25;
• excess MT — ?25 <30;
• Grade I obesity — ?30 <35;
• Grade II obesity — ?35 <40;
• obesity of the III degree — ?40.
BMI <18.5 is characterized as a body weight deficit.
The distribution of adipose tissue plays an important role. There are two types of obesity:
•gynoid (of the "pear" type), when excess adipose tissue is distributed mainly on the hips and buttocks;
•android (like "apple"; abdominal obesity), with predominant localization of fat in the upper half of the body (abdomen, chest, shoulders, back).
The second type of obesity is more pathogenic in terms of the risk of cardiovascular diseases and diabetes mellitus. This is due to obesity of internal organs, including the liver (visceral obesity, non-alcoholic fatty liver disease), a decrease in blood oxygen saturation due to the transition of respiration to the thoracic, superficial type and endocrine activity of visceral adipose tissue with a pathological change in the production of adipokines (leptin, ghrelin, adiponectin). A clear correlation was found between an increase in abdominal adipose tissue and body mass index with the risk of concomitant diseases. It is believed that the risks begin to increase with an increase in waist circumference (FROM) >80 cm in women and 94 cm in men, and with >88 cm and 102 cm, respectively, the risk increases significantly.
The central pathological link of the metabolic syndrome is a change in carbohydrate metabolism. Glucose concentration is estimated in capillary plasma (norm < 5.6) and in venous plasma (norm <6.1) on an empty stomach in mmol / L. Fasting hyperglycemia is characterized by ?5.6 <6.1 and ?6.1; <7.0; diabetes mellitus — ?6.1 and ?6.1 <7.0, respectively. 2 hours after taking a carbohydrate load (75 g of glucose or 125 g of refined sugar dissolved in 200 ml of water), the normal glucose concentration in capillary and venous blood is <7.8 mmol/l; HTG is ?7.8 <11.1 and diabetes mellitus is ?11.1.
Another important component of the metabolic syndrome is arterial hypertension, which may be secondary in nature. Systolic blood pressure (SBP) of 120-129 mmHg is considered normal BP and diastolic blood pressure (DBP) of 80-84 mmHg. SBP <120 and DBP <80 are called optimal blood pressure, and SBP 130-139 and DBP 85-89 are called high normal blood pressure. There are three degrees of arterial hypertension:
•1 st. – SAD 140-159, DAD 90-99;
•2 st. - GARDEN 160-179, DAD 100-109;
•3 st. - SAD ?180, DAD ?110.
An increase in blood pressure is characterized by an increased risk of cardiovascular events.
Metabolic syndrome is also characterized by changes in lipid metabolism, which are classified in the table below (in mmol/l).
Metabolic syndrome in women of reproductive age was previously known by practitioners as neurotransmission endocrine syndrome, occurring as a mild form of Cushing's disease, hypothalamic or diencephalic syndrome. In this article, the material will be presented from the perspective of a gynecologist- endocrinologist. In women of reproductive age, metabolic syndrome is one of the most common causes of reproductive dysfunction against the background of progressive obesity and diencephalic symptoms.
EPIDEMIOLOGY
The frequency of this pathology is up to 15- 20% in the population, about 30-35% in the structure of reproductive disorders and up to 70% among women with recurrent endometrial hyperplastic processes; the frequency of early pregnancy losses in this syndrome increases to 35%.
ETIOLOGY
The causes of the development of metabolic syndrome are the effects of various factors (mental stress, neuroinfections, various operations, injuries, childbirth, abortions, etc.) in women with a certain premorbid background (congenital or acquired functional lability of hypothalamic and extrahypothalamic structures).
PATHOGENESIS
Primarily, there is a violation of the neuroendocrine regulation of the hypothalamus, therefore, there are many diencephalic symptoms (sleep disorders, appetite, thirst, dizziness, headaches, hypertension, etc.), indicating the central (hypothalamic) genesis of this pathology. In response to the effects of various etiological factors (stress), neurotransmitter metabolism is disrupted in the extrahypothalamic structures of the brain, in particular, an increase in the synthesis and release of ?- endorphin and a decrease in dopamine production.
As a result, the secretion of ACSH (adrenocorticosteroid hormone) and prolactin increases, and the cyrhoral rhythm of gonadoliberin and, accordingly, gonadotropins in the pituitary gland is disrupted. Estrone, which is non-gonadally synthesized from androgens, increases the sensitivity of the pituitary gland to gonadoliberin, which additionally disrupts the function of the hypothalamic-pituitary- ovarian system with the formation of secondary polycystic ovaries.
Disorders in the hypothalamus-pituitary- adrenal gland system. In response to excessive stimulation of ACSH in the adrenal glands, the formation of all steroid hormones of the cortex increases: glucocorticoids (cortisol), mineralocorticoids (aldosterone) and sex hormones, mainly androgens.
Hypercorticism contributes to specific, so- called visceral obesity (central, cushingoid, male, android obesity) with predominant deposition of adipose tissue in the shoulder girdle, abdomen and mesentery of internal organs.
Visceral adipose tissue leads to the formation of insulin resistance due to hyperinsulinemia. Then there is a violation of the blood lipid spectrum (dyslipidemia), characterized by an increase in the level of atherogenic factors (triglycerides, low-density lipoproteins, very low-density lipoproteins) and a decrease in the level of high-density lipoproteins, which leads to atherosclerosis and arterial hypertension. In this case, the sequence of development of metabolic disorders corresponds to the duration of the disease.
Therefore, arterial hypertension, an obligatory component of the metabolic syndrome, usually manifests itself after the age of 35.
Visceral obesity is also promoted by bulimia (increased appetite and excessive food intake) due to impaired neurotransmitter control over the function of the centers of eating behavior located in the hypothalamus. Peripheral insulin resistance is also promoted by adrenal androgens and testosterone produced in adipose tissue. Androgens are known to alter the structure of muscle tissue towards the predominance of type II muscle fibers, which are less sensitive to insulin.
Thus, as a result of activation of the hypothalamus-pituitary-adrenal axis, 4 main components ("deadly quartet") of the metabolic syndrome are formed: visceral obesity, insulin resistance, dyslipidemia and arterial hypertension.
There is no clear classification and staging of the metabolic syndrome. Despite this, the severity of symptoms, the number of components of Raven syndrome and the presence of complications influence the risk stratification and the choice of treatment tactics in a particular patient. To do this, consider:
• the degree of obesity and hypertension;
• severity of metabolic changes;
• the presence or absence of diabetes mellitus and atherosclerosis-related diseases.
Depending on the body mass index (BMI), which is calculated by dividing weight (kg) by height (m2), the following types of body weight (MT) are classified:
• normal MT — BMI ?18.5 <25;
• excess MT — ?25 <30;
• Grade I obesity — ?30 <35;
• Grade II obesity — ?35 <40;
• obesity of the III degree — ?40.
BMI <18.5 is characterized as a body weight deficit.
The distribution of adipose tissue plays an important role. There are two types of obesity:
•gynoid (of the "pear" type), when excess adipose tissue is distributed mainly on the hips and buttocks;
•android (like "apple"; abdominal obesity), with predominant localization of fat in the upper half of the body (abdomen, chest, shoulders, back).
The second type of obesity is more pathogenic in terms of the risk of cardiovascular diseases and diabetes mellitus. This is due to obesity of internal organs, including the liver (visceral obesity, non-alcoholic fatty liver disease), a decrease in blood oxygen saturation due to the transition of respiration to the thoracic, superficial type and endocrine activity of visceral adipose tissue with a pathological change in the production of adipokines (leptin, ghrelin, adiponectin). A clear correlation was found between an increase in abdominal adipose tissue and body mass index with the risk of concomitant diseases. It is believed that the risks begin to increase with an increase in waist circumference (FROM) >80 cm in women and 94 cm in men, and with >88 cm and 102 cm, respectively, the risk increases significantly.
The central pathological link of the metabolic syndrome is a change in carbohydrate metabolism. Glucose concentration is estimated in capillary plasma (norm < 5.6) and in venous plasma (norm <6.1) on an empty stomach in mmol / L. Fasting hyperglycemia is characterized by ?5.6 <6.1 and ?6.1; <7.0; diabetes mellitus — ?6.1 and ?6.1 <7.0, respectively. 2 hours after taking a carbohydrate load (75 g of glucose or 125 g of refined sugar dissolved in 200 ml of water), the normal glucose concentration in capillary and venous blood is <7.8 mmol/l; HTG is ?7.8 <11.1 and diabetes mellitus is ?11.1.
Another important component of the metabolic syndrome is arterial hypertension, which may be secondary in nature. Systolic blood pressure (SBP) of 120-129 mmHg is considered normal BP and diastolic blood pressure (DBP) of 80-84 mmHg. SBP <120 and DBP <80 are called optimal blood pressure, and SBP 130-139 and DBP 85-89 are called high normal blood pressure. There are three degrees of arterial hypertension:
•1 st. – SAD 140-159, DAD 90-99;
•2 st. - GARDEN 160-179, DAD 100-109;
•3 st. - SAD ?180, DAD ?110.
An increase in blood pressure is characterized by an increased risk of cardiovascular events.
Metabolic syndrome is also characterized by changes in lipid metabolism, which are classified in the table below (in mmol/l).
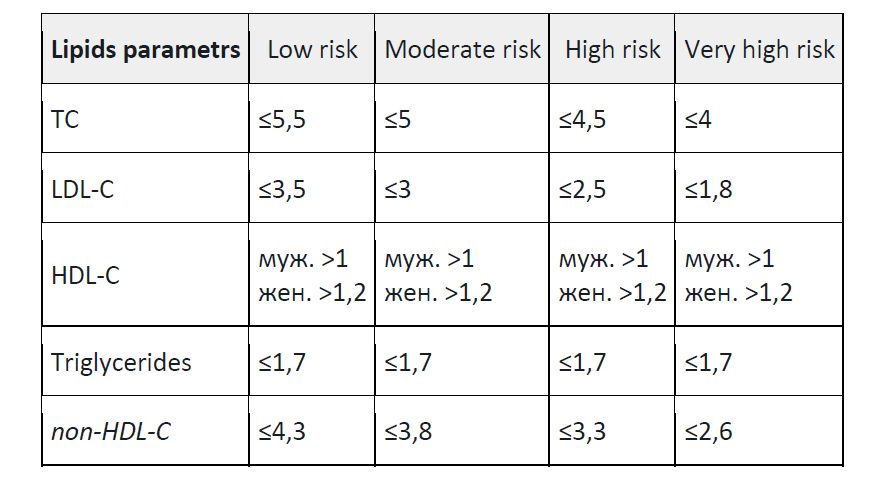
Note:
TC - total cholesterol;
LDL-C, low-density lipoprotein cholesterol;
HDL-C, high-density lipoprotein cholesterol;
non-HDL-C, non-high-density lipoprotein cholesterol.
The role of insulin in ovarian function in women is reduced to an increase in LH- dependent testosterone synthesis. In addition, insulin suppresses the production of SHBG (globulin, which binds sex hormones) in the liver, thereby increasing the level of biologically active free fractions of testosterone and estradiol in the blood. Hyperinsulinemia reduces the production of proteins in the liver that bind insulin-like growth factor, which leads to increased bioavailability of insulin-like growth factor, which, like insulin, enhances the synthesis of androgens in ovarian teca cells. All these mechanisms ultimately exacerbate hyperandrogenism.
Hypothalamic-pituitary-ovarian system. In women with metabolic syndrome, polycystic ovaries are formed not only due to metabolic disorders, but also due to a primary violation of neurotransmitter control over gonadoliberin function. The mechanisms of formation of secondary polycystic ovaries can be simplified as follows. As a result of changes in gonadoliberin secretion, gonadotropin production is disrupted towards an increase in LH levels and a relative decrease in FSH synthesis. Ovulation is disrupted in the ovaries, first the persistence of follicles occurs, then their atresia. An excess of androgens is produced in atretic follicles and estradiol deficiency occurs. According to negative feedback mechanisms, a decrease in estradiol concentration stimulates excessive LH production. Ovarian androgens aggravate the process of cystic follicle atresia, contribute to hyperplasia of teca cells and stroma, as well as thickening of the protein membrane of the ovaries.
An excess of androgens primarily from the adrenal glands, and then from polycystic ovaries in adipose tissue increases the synthesis of estrone. High concentrations of extra-gonadal estrone increase the sensitivity of the pituitary gland to gonadoliberin, which leads to chronic hypersecretion of LH and closes the "vicious circle" in the formation of secondary polycystic ovaries.
THE CLINICAL PICTURE
The cardinal sign of metabolic syndrome in women is a violation of menstrual and generative function against the background of a 10-30 kg body weight gain. Mostly, patients complain of menstrual irregularities, miscarriage, infertility, excessive hair loss, obesity and a variety of "diencephalic complaints". Moreover, the patient's overweight is associated with endocrine disorders, and not with alimentary factors. Only with a carefully collected medical history can the presence of increased appetite, the main factor of obesity, be revealed.
In men, metabolic syndrome often develops after the age of 45 due to a decrease in testosterone levels. Against the background of hormone deficiency, weight increases, insulin metabolism is disrupted, and blood pressure rises.
The consequences of metabolic syndrome in men include:
•Atherosclerotic vascular disease
•Obesity
•Prediabetes
•Erectile dysfunction. The pathology is caused by atherosclerotic lesions of the vessels and arteries that feed the testicles and prostate gland. In men, this is expressed in a decrease in the duration of erection, early ejaculation, loss of sensitivity of the glans penis. In Europe, 1-2 sexual acts per week are considered normal for people over the age of 60. Many couples over the age of 40 have sex several times a month. At the same time, the quality of sex does not leave satisfaction, provoking dissatisfaction with family life and a partner.
•Prostate cancer. The prostate performs a number of functions: it retains urine, produces ejaculate, and processes testosterone. When there is a lack of hormone, the cells become inactive and mutate over time. Excess testosterone also has a negative effect on the prostate gland, and also provokes cancer. But cancer cells in the latter case are less aggressive, and after surgery and chemotherapy, the patient has a better chance of a full recovery. With testosterone deficiency, mutated cells quickly metastasize and are practically resistant to chemotherapy).
•Osteoporosis and bone fragility. Testosterone affects bone density. The hormone provokes the production of osteoblasts — young bone cells. It also supports the mineral composition of bones. With a decrease in testosterone, there is a risk of fractures, bone tissue becomes more porous.
Excess cholesterol, formed due to a decrease in testosterone production, settles on the
vessels of the heart and brain. The death of a young man aged 30-35 after a heart attack comes as a shock to his relatives. Metabolic syndrome and an early decrease in androgenic hormones are often hereditary, so it can be predicted and cured.
DIAGNOSTICS
The diagnosis of metabolic syndrome is based on clinical data and phenotypic features (menstrual cycle disorders, against the background of weight gain, android obesity and "diencephalic" complaints).
ANAMNESIS
Of the transferred diseases, there is a high incidence of acute respiratory viral infections various extragenital pathologies. Heredity in most patients is burdened with reproductive disorders, obesity, insulin-dependent diabetes mellitus, and cardiovascular diseases. At the same time, it is necessary to identify factors contributing to weight gain in order to determine the duration of the disease and the likelihood of the formation of secondary signs. Menstrual and generative function in women: the age of menarche does not differ from that in the population — 12-13 years. A distinctive feature is a secondary violation of the menstrual cycle after exposure to various factors against the background of weight gain. Menstrual cycle disorders begin with an increase in cycle duration, NFD (luteal phase deficiency), and then oligoamenorrhea and chronic anovulation develop; the frequency of dysfunctional uterine bleeding is up to 20%. Since most patients had a history of pregnancies that ended in childbirth, abortions, a violation of generative function is more often characterized by secondary infertility or miscarriage (at the beginning of the disease).
PHYSICAL EXAMINATION
In physical examination, the body mass index corresponds to obesity and is over 30, and the ratio of waist circumference to hip circumference is characteristic of the visceral type of obesity (more than 0.85). An important clinical sign is stretch marks on the skin of the abdomen, thighs, from pale pink to purple. Skin changes of the "nigroid acanthosis" type are often observed, in the form of rough pigmented skin areas in places of friction and folds (inguinal, axillary, under the mammary glands, on the abdomen).
These skin changes indicate insulin resistance. The severity of hirsutism and acne in women is higher than in PCOS, which is due to the influence of not only adrenal androgens, but also extra-gonadally synthesized testosterone in a large amount of adipose tissue. During the formation of secondary polycystic ovaries, the growth of taper hair increases not only along the white line of the abdomen, periarticular margins and inner surface of the thighs, but also often in the chin, sideburns, sternum, back, buttocks. At the same time, some patients have signs of virile syndrome — androgen- dependent alopecia and a decrease in voice timbre. The condition of the mammary glands is characterized by their hypertrophy due to adipose tissue and a high frequency of fibrocystic mastopathy. During gynecological examination, it is necessary to pay attention to the degree of estrogenic saturation in the cervical number, which is 10-12 cm in the first phase of the disease, and 5-6 cm in the formation of secondary polycystic ovaries. In addition, in these patients, "nigroid acanthosis" is most often observed in the inguinal folds.
In addition to abdominal obesity, it is necessary to have at least two additional criteria for diagnosis:
•arterial hypertension (blood pressure ?140/90 mmHg);
•lipid parameters (mmol/l) — an increase in the concentration of triglycerides in the blood ?1.7; a decrease in HDL cholesterol <1.0 in men; <1.2 in women and an increase in LDL cholesterol >3.0;
•carbohydrate indices (mmol/l) — fasting hyperglycemia ?6.1 and HTG 7.8 – <11.1
In clinical settings, it is necessary to differentiate the metabolic syndrome from a mechanical combination of risk factors, such as hypertension, overweight without signs of abdominal obesity and increased blood total cholesterol levels, which is quite common (up to 30%). In doubtful cases, additional determination of insulin resistance is recommended using the following methods:
•assessment of basal hyperinsulinemia in fasting blood (hyperinsulinemia — >18 µed/ml);
•the HOMA-IR indicator is the product of the fasting insulin value (µed/ml) by the glucose value (mmol/l), divided by 22.5 (a value greater than 2.27 is considered insulin resistance);
•Caro index — the ratio of lean glucose (in mmol/l) to insulin (in µed/ml) (insulin resistance – value < 0.33)
INSTRUMENTAL RESEARCH
Metabolic disorders are characterized by insulin resistance and, as a result, hyperinsulinemia, dyslipidemia (increased low-density lipoproteins, triglycerides, decreased levels of high-density lipoproteins). An oral glucose tolerance test with the determination of basal and glucose- stimulated concentrations of insulin and glucose reveals a violation of glucose tolerance. The peak of insulinemia is observed after 60 minutes, and after 120 minutes, insulin (but not glucose) indicators reach the initial or slightly higher reference values. In addition, the laboratory criteria for insulin resistance are a basal insulin concentration of 12.2 mMU/l or more. The definition of the HOMA index, whose value of more than 2.5 indicates insulin resistance, can also be considered informative. To calculate this index, only the values of the basal concentrations of glucose and insulin are needed, which are multiplied and divided by 22.5.
Transvaginal echography in women will help identify secondary polycystic ovaries. At the beginning of the disease, multifollicular ovaries are determined, which differ in the normal volume of the stroma with many follicles up to 10-12 mm in diameter.
LABORATORY TESTS
Hormonal studies are characterized by an increase in the concentration of ACSH, cortisol, and prolactin in the blood. The level of LH and FSH may be normal, and with the formation of secondary polycystic ovaries in women, the concentration of LH increases with an increase in the LH/FSH ratio to 2.5–3. Insulin levels are also increased and SHBG (sex hormone binding globulin) levels are reduced. In addition, an increase in the blood content of 17-OP, testosterone and DHEA is characteristic. This often leads to the unjustified prescription of dexamethasone for adrenal hyperandrogenism, which is pathogenetically unjustified in hypercorticism, since these patients already have an increased concentration of cortisol.
Endometrial biopsy shows a high frequency of hyperplastic processes and adenomatosis in the endometrium (up to 60%), which is undoubtedly associated with pronounced metabolic disorders. Therefore, practitioners should treat these patients with oncological caution and recommend separate curettage for menstrual disorders, as well as echographic signs of endometrial hyperplasia.
DIFFERENTIAL DIAGNOSIS
Differential diagnosis is carried out primarily with Cushing's disease. The diagnosis requires the participation of general endocrinologists, for whom Cushing's disease is not uncommon. At the same time, there are high levels of ACTH, cortisol and prolactin and echographic signs of adrenal cortex hyperplasia. Differential diagnosis in women is also carried out with a special pathology of the ovaries — stromal tecamatosis.
The clinical picture of this pathology is characterized by obesity, pronounced virile syndrome with "nigroid acanthosis" and insulin resistance. The level of androgens in the blood is significantly increased with normal levels of LH and FSH, the size of the ovaries may be normal. A characteristic feature is recurrent hyperplastic endometrial processes that are not amenable to hormone therapy. Differential diagnosis with PCOS and obesity is most often necessary. In this case, the main role is assigned to the data of anamnesis (the secondary nature of menstrual and generative function disorders against the background of metabolic syndrome), since the echographic, endocrinological and metabolic characteristics do not differ from those in PCOS with obesity during the formation of secondary polycystic ovaries.
TREATMENT
Treatment presents certain difficulties, since the restoration of hormonal and generative function can be achieved only against the background of normalization of body weight. The most common mistake of practicing doctors is hormone therapy against the background of obesity. Early detection of the disease at the stage of functional disorders,
before the formation of serious complications, is important. In this case, metabolic therapy leads to the restoration of normal blood pressure, normalization of blood parameters, restoration of reproductive and sexual function in patients of both sexes.
TREATMENT GOALS
The main goal of treatment is normalization of body weight, restoration of metabolic and hormonal homeostasis, which contributes not only to the realization of generative function, but also to reducing health risks, developing long—term healthy lifestyle skills. Rational nutrition implies a decrease in energy value due to fats and carbohydrates and is the basis of metabolic therapy.
The duration of metabolic therapy is 6 months or more, depending on the initial body weight and the rate of its decrease.
After weight loss, ovulatory menstrual cycle and fertility are restored in some women, since secondary polycystic ovaries have not yet formed. During the period of normalization of body weight, it is recommended to protect against pregnancy, which may be complicated by severe gestosis or interrupted in the early stages.
Anovulation after normalization of body weight and metabolic disorders indicates the formation of secondary polycystic ovaries. In this case, it is recommended to stimulate ovulation conservatively or surgically. Since infertility is more often secondary, before ovulation stimulation, it is necessary to exclude the tubal factor.
The multifactorial pathogenesis of metabolic syndrome involving many systems in the body causes the complexity and low effectiveness of therapy, the basis of which should be the regulation of neurotransmitter metabolism of the central nervous system against the background of normalization of body weight, especially in the formation of complications. Timely correction of metabolic disorders at the first (functional) stage of the disease is more effective in restoring reproductive health and preventing the development of cardiovascular diseases, insulin— independent diabetes mellitus - the consequences of metabolic syndrome that worsen people's quality of life.
TC - total cholesterol;
LDL-C, low-density lipoprotein cholesterol;
HDL-C, high-density lipoprotein cholesterol;
non-HDL-C, non-high-density lipoprotein cholesterol.
The role of insulin in ovarian function in women is reduced to an increase in LH- dependent testosterone synthesis. In addition, insulin suppresses the production of SHBG (globulin, which binds sex hormones) in the liver, thereby increasing the level of biologically active free fractions of testosterone and estradiol in the blood. Hyperinsulinemia reduces the production of proteins in the liver that bind insulin-like growth factor, which leads to increased bioavailability of insulin-like growth factor, which, like insulin, enhances the synthesis of androgens in ovarian teca cells. All these mechanisms ultimately exacerbate hyperandrogenism.
Hypothalamic-pituitary-ovarian system. In women with metabolic syndrome, polycystic ovaries are formed not only due to metabolic disorders, but also due to a primary violation of neurotransmitter control over gonadoliberin function. The mechanisms of formation of secondary polycystic ovaries can be simplified as follows. As a result of changes in gonadoliberin secretion, gonadotropin production is disrupted towards an increase in LH levels and a relative decrease in FSH synthesis. Ovulation is disrupted in the ovaries, first the persistence of follicles occurs, then their atresia. An excess of androgens is produced in atretic follicles and estradiol deficiency occurs. According to negative feedback mechanisms, a decrease in estradiol concentration stimulates excessive LH production. Ovarian androgens aggravate the process of cystic follicle atresia, contribute to hyperplasia of teca cells and stroma, as well as thickening of the protein membrane of the ovaries.
An excess of androgens primarily from the adrenal glands, and then from polycystic ovaries in adipose tissue increases the synthesis of estrone. High concentrations of extra-gonadal estrone increase the sensitivity of the pituitary gland to gonadoliberin, which leads to chronic hypersecretion of LH and closes the "vicious circle" in the formation of secondary polycystic ovaries.
THE CLINICAL PICTURE
The cardinal sign of metabolic syndrome in women is a violation of menstrual and generative function against the background of a 10-30 kg body weight gain. Mostly, patients complain of menstrual irregularities, miscarriage, infertility, excessive hair loss, obesity and a variety of "diencephalic complaints". Moreover, the patient's overweight is associated with endocrine disorders, and not with alimentary factors. Only with a carefully collected medical history can the presence of increased appetite, the main factor of obesity, be revealed.
In men, metabolic syndrome often develops after the age of 45 due to a decrease in testosterone levels. Against the background of hormone deficiency, weight increases, insulin metabolism is disrupted, and blood pressure rises.
The consequences of metabolic syndrome in men include:
•Atherosclerotic vascular disease
•Obesity
•Prediabetes
•Erectile dysfunction. The pathology is caused by atherosclerotic lesions of the vessels and arteries that feed the testicles and prostate gland. In men, this is expressed in a decrease in the duration of erection, early ejaculation, loss of sensitivity of the glans penis. In Europe, 1-2 sexual acts per week are considered normal for people over the age of 60. Many couples over the age of 40 have sex several times a month. At the same time, the quality of sex does not leave satisfaction, provoking dissatisfaction with family life and a partner.
•Prostate cancer. The prostate performs a number of functions: it retains urine, produces ejaculate, and processes testosterone. When there is a lack of hormone, the cells become inactive and mutate over time. Excess testosterone also has a negative effect on the prostate gland, and also provokes cancer. But cancer cells in the latter case are less aggressive, and after surgery and chemotherapy, the patient has a better chance of a full recovery. With testosterone deficiency, mutated cells quickly metastasize and are practically resistant to chemotherapy).
•Osteoporosis and bone fragility. Testosterone affects bone density. The hormone provokes the production of osteoblasts — young bone cells. It also supports the mineral composition of bones. With a decrease in testosterone, there is a risk of fractures, bone tissue becomes more porous.
Excess cholesterol, formed due to a decrease in testosterone production, settles on the
vessels of the heart and brain. The death of a young man aged 30-35 after a heart attack comes as a shock to his relatives. Metabolic syndrome and an early decrease in androgenic hormones are often hereditary, so it can be predicted and cured.
DIAGNOSTICS
The diagnosis of metabolic syndrome is based on clinical data and phenotypic features (menstrual cycle disorders, against the background of weight gain, android obesity and "diencephalic" complaints).
ANAMNESIS
Of the transferred diseases, there is a high incidence of acute respiratory viral infections various extragenital pathologies. Heredity in most patients is burdened with reproductive disorders, obesity, insulin-dependent diabetes mellitus, and cardiovascular diseases. At the same time, it is necessary to identify factors contributing to weight gain in order to determine the duration of the disease and the likelihood of the formation of secondary signs. Menstrual and generative function in women: the age of menarche does not differ from that in the population — 12-13 years. A distinctive feature is a secondary violation of the menstrual cycle after exposure to various factors against the background of weight gain. Menstrual cycle disorders begin with an increase in cycle duration, NFD (luteal phase deficiency), and then oligoamenorrhea and chronic anovulation develop; the frequency of dysfunctional uterine bleeding is up to 20%. Since most patients had a history of pregnancies that ended in childbirth, abortions, a violation of generative function is more often characterized by secondary infertility or miscarriage (at the beginning of the disease).
PHYSICAL EXAMINATION
In physical examination, the body mass index corresponds to obesity and is over 30, and the ratio of waist circumference to hip circumference is characteristic of the visceral type of obesity (more than 0.85). An important clinical sign is stretch marks on the skin of the abdomen, thighs, from pale pink to purple. Skin changes of the "nigroid acanthosis" type are often observed, in the form of rough pigmented skin areas in places of friction and folds (inguinal, axillary, under the mammary glands, on the abdomen).
These skin changes indicate insulin resistance. The severity of hirsutism and acne in women is higher than in PCOS, which is due to the influence of not only adrenal androgens, but also extra-gonadally synthesized testosterone in a large amount of adipose tissue. During the formation of secondary polycystic ovaries, the growth of taper hair increases not only along the white line of the abdomen, periarticular margins and inner surface of the thighs, but also often in the chin, sideburns, sternum, back, buttocks. At the same time, some patients have signs of virile syndrome — androgen- dependent alopecia and a decrease in voice timbre. The condition of the mammary glands is characterized by their hypertrophy due to adipose tissue and a high frequency of fibrocystic mastopathy. During gynecological examination, it is necessary to pay attention to the degree of estrogenic saturation in the cervical number, which is 10-12 cm in the first phase of the disease, and 5-6 cm in the formation of secondary polycystic ovaries. In addition, in these patients, "nigroid acanthosis" is most often observed in the inguinal folds.
In addition to abdominal obesity, it is necessary to have at least two additional criteria for diagnosis:
•arterial hypertension (blood pressure ?140/90 mmHg);
•lipid parameters (mmol/l) — an increase in the concentration of triglycerides in the blood ?1.7; a decrease in HDL cholesterol <1.0 in men; <1.2 in women and an increase in LDL cholesterol >3.0;
•carbohydrate indices (mmol/l) — fasting hyperglycemia ?6.1 and HTG 7.8 – <11.1
In clinical settings, it is necessary to differentiate the metabolic syndrome from a mechanical combination of risk factors, such as hypertension, overweight without signs of abdominal obesity and increased blood total cholesterol levels, which is quite common (up to 30%). In doubtful cases, additional determination of insulin resistance is recommended using the following methods:
•assessment of basal hyperinsulinemia in fasting blood (hyperinsulinemia — >18 µed/ml);
•the HOMA-IR indicator is the product of the fasting insulin value (µed/ml) by the glucose value (mmol/l), divided by 22.5 (a value greater than 2.27 is considered insulin resistance);
•Caro index — the ratio of lean glucose (in mmol/l) to insulin (in µed/ml) (insulin resistance – value < 0.33)
INSTRUMENTAL RESEARCH
Metabolic disorders are characterized by insulin resistance and, as a result, hyperinsulinemia, dyslipidemia (increased low-density lipoproteins, triglycerides, decreased levels of high-density lipoproteins). An oral glucose tolerance test with the determination of basal and glucose- stimulated concentrations of insulin and glucose reveals a violation of glucose tolerance. The peak of insulinemia is observed after 60 minutes, and after 120 minutes, insulin (but not glucose) indicators reach the initial or slightly higher reference values. In addition, the laboratory criteria for insulin resistance are a basal insulin concentration of 12.2 mMU/l or more. The definition of the HOMA index, whose value of more than 2.5 indicates insulin resistance, can also be considered informative. To calculate this index, only the values of the basal concentrations of glucose and insulin are needed, which are multiplied and divided by 22.5.
Transvaginal echography in women will help identify secondary polycystic ovaries. At the beginning of the disease, multifollicular ovaries are determined, which differ in the normal volume of the stroma with many follicles up to 10-12 mm in diameter.
LABORATORY TESTS
Hormonal studies are characterized by an increase in the concentration of ACSH, cortisol, and prolactin in the blood. The level of LH and FSH may be normal, and with the formation of secondary polycystic ovaries in women, the concentration of LH increases with an increase in the LH/FSH ratio to 2.5–3. Insulin levels are also increased and SHBG (sex hormone binding globulin) levels are reduced. In addition, an increase in the blood content of 17-OP, testosterone and DHEA is characteristic. This often leads to the unjustified prescription of dexamethasone for adrenal hyperandrogenism, which is pathogenetically unjustified in hypercorticism, since these patients already have an increased concentration of cortisol.
Endometrial biopsy shows a high frequency of hyperplastic processes and adenomatosis in the endometrium (up to 60%), which is undoubtedly associated with pronounced metabolic disorders. Therefore, practitioners should treat these patients with oncological caution and recommend separate curettage for menstrual disorders, as well as echographic signs of endometrial hyperplasia.
DIFFERENTIAL DIAGNOSIS
Differential diagnosis is carried out primarily with Cushing's disease. The diagnosis requires the participation of general endocrinologists, for whom Cushing's disease is not uncommon. At the same time, there are high levels of ACTH, cortisol and prolactin and echographic signs of adrenal cortex hyperplasia. Differential diagnosis in women is also carried out with a special pathology of the ovaries — stromal tecamatosis.
The clinical picture of this pathology is characterized by obesity, pronounced virile syndrome with "nigroid acanthosis" and insulin resistance. The level of androgens in the blood is significantly increased with normal levels of LH and FSH, the size of the ovaries may be normal. A characteristic feature is recurrent hyperplastic endometrial processes that are not amenable to hormone therapy. Differential diagnosis with PCOS and obesity is most often necessary. In this case, the main role is assigned to the data of anamnesis (the secondary nature of menstrual and generative function disorders against the background of metabolic syndrome), since the echographic, endocrinological and metabolic characteristics do not differ from those in PCOS with obesity during the formation of secondary polycystic ovaries.
TREATMENT
Treatment presents certain difficulties, since the restoration of hormonal and generative function can be achieved only against the background of normalization of body weight. The most common mistake of practicing doctors is hormone therapy against the background of obesity. Early detection of the disease at the stage of functional disorders,
before the formation of serious complications, is important. In this case, metabolic therapy leads to the restoration of normal blood pressure, normalization of blood parameters, restoration of reproductive and sexual function in patients of both sexes.
TREATMENT GOALS
The main goal of treatment is normalization of body weight, restoration of metabolic and hormonal homeostasis, which contributes not only to the realization of generative function, but also to reducing health risks, developing long—term healthy lifestyle skills. Rational nutrition implies a decrease in energy value due to fats and carbohydrates and is the basis of metabolic therapy.
The duration of metabolic therapy is 6 months or more, depending on the initial body weight and the rate of its decrease.
After weight loss, ovulatory menstrual cycle and fertility are restored in some women, since secondary polycystic ovaries have not yet formed. During the period of normalization of body weight, it is recommended to protect against pregnancy, which may be complicated by severe gestosis or interrupted in the early stages.
Anovulation after normalization of body weight and metabolic disorders indicates the formation of secondary polycystic ovaries. In this case, it is recommended to stimulate ovulation conservatively or surgically. Since infertility is more often secondary, before ovulation stimulation, it is necessary to exclude the tubal factor.
The multifactorial pathogenesis of metabolic syndrome involving many systems in the body causes the complexity and low effectiveness of therapy, the basis of which should be the regulation of neurotransmitter metabolism of the central nervous system against the background of normalization of body weight, especially in the formation of complications. Timely correction of metabolic disorders at the first (functional) stage of the disease is more effective in restoring reproductive health and preventing the development of cardiovascular diseases, insulin— independent diabetes mellitus - the consequences of metabolic syndrome that worsen people's quality of life.